Last week, I talked about yinyang theory as a central element of classical Chinese philosophy and a powerful modern analytical tool. Yin and yang and their delicate, dynamic balance help to understand the vicissitudes of the natural world and the pains and processes of the human body. These concepts are, of course, not without their own history. Through the course of classical Chinese history, yin and yang developed through Chinese thinkers’ observations of the natural world. Later, yin and yang merged with other philosophical worldviews, and came to inhere in the body and its various organ systems. In the past century, yin and yang found resonance with Western philosophies of contradiction and resolution, particularly Marxist and Hegelian dialectics. There’s so much history, so much philosophy, so many years of medical practice behind those two words, pushing and pulling yin and yang into their modern shape. It’s pretty mind-blowing. (And we haven’t even gotten to qi, or meridians, or organ systems yet!)
So what happens in the clinic? How does all this theory fit into the everyday practice of treating disease?
On two mornings each week, I spend up to four hours in a small, sometimes cramped and stuffy room, observing the clinical practice of TCM. I shadow a TCM gynecology clinic on Wednesdays; on Fridays, I’m in my professor’s expert clinic, which receives patients suffering from diabetes, high blood pressure, and more.
While the clinics are located in different hospitals, the rooms have a similar layout. The physician, patient, and sometimes a graduate student or two sit at a table in the center of the room, with a computer and printer within reach. (On Fridays, when the modestly sized room must fit up to 12 occupants, including four to six graduate students, two or three other shadowers, and upcoming patients, people stand, sit on stools, and pile onto an examination bed pushed against one wall.) The computer is central to the consultation process: the hospital database holds the patient’s medical history and allows the doctor to input diagnoses and prescriptions. The doctor will look at the patient’s tongue, take their pulse, and discuss their recent state of bodily health. Along these broader dimensions, clinical TCM seems largely unremarkable, and surprisingly similar to biomedicine.
But the pulse TCM physicians are concerned with is a different pulse from the one you can measure with a cuff. The tongue tells them more information about the patient’s wellbeing than a biomedical professional might be able to glean. And even in moments when biomedicine and TCM visibly collide — when the gynecologist orders a pap smear or a B ultrasound, when the patient brings in the results from a recent blood test or CT scan, or when a diagnosis of diabetes looms — the theory of TCM remains, marking this clinic as a place where the ideas, entities, and approaches that figure into illness and treatment exceed biomedicine, even if they do not by any means exclude it.
Let’s take an example from the gynecology clinic. Many of the women who seek medical help are going through menopause. As the physician I shadow (who I’ll call Dr. G) points out, the symptoms these women report might be lightly overlooked by a biomedical doctor, or earn a prescription for hormonal regulation. The former can be immensely unsatisfying, resigning the patient to a host of pressing discomforts with little palliative assistance; the latter, while it addresses the patient’s complains, brings with it a host of potential side effects. TCM approaches the issue differently.
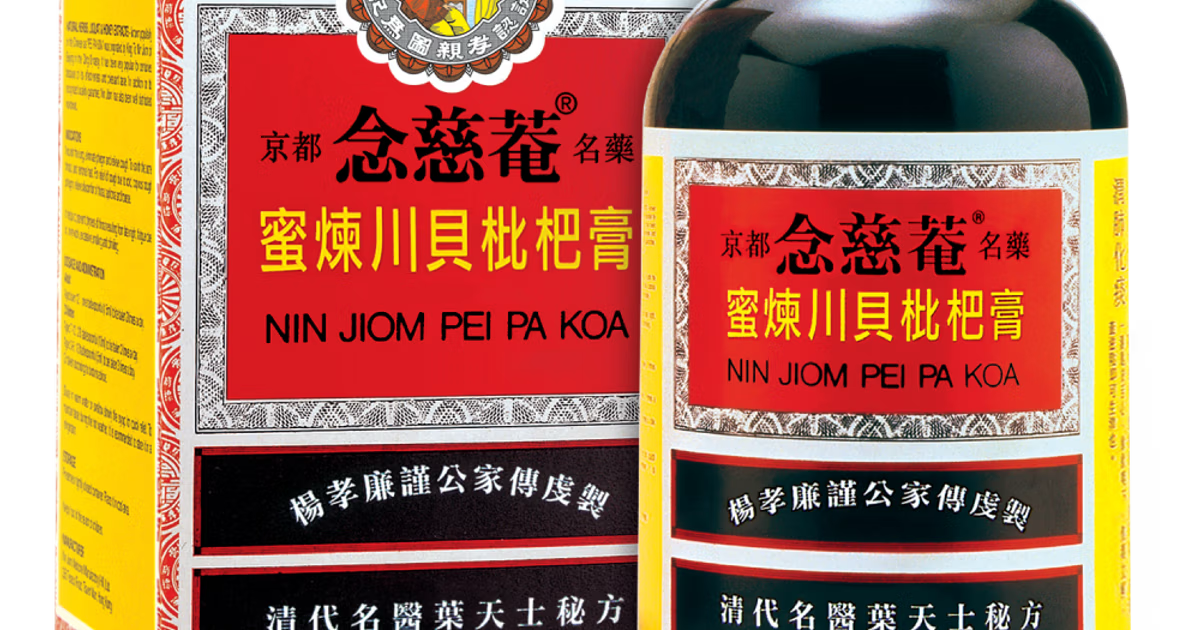
The 黄帝内经 (Huangdi Neijing, in English: Inner Canon of the Yellow Emperor, China’s oldest and most essential medical text, more than two thousand years old) divides a woman’s lifespan into periods of seven years; each period marks a different phase in her growth, aging, and reproductive health. Menopause coincides with七七 qiqi (seven-seven), the period of seven years beginning at age 49. During this time, kidney qi (literally, air, breath; or “vital energy”) is declining, and it’s easy for the body’s yin and yang to lose balance and fall out of order. By listening to the patient’s particular complaints and collecting additional data on the state of her organ systems through pulse-taking and checking the size, color, and coating of her tongue, Dr. G can figure out what sort of herbs might address each patient’s needs. Her prescriptions — which are largely based off of classical formulae improved through generations’ worth of innovation, tailored to suit the individual patient — usually contain 12-15 herbs, each with a particular curative effect, that work together to readjust the patient’s yinyang balance and support the function of her organ systems. Classical medical theory — the Huangdi Neijing, yin and yang, a belief that bodily organs can’t be reduced to an anatomical organ we can remove, dissect, or transplant — looms large throughout this process, even as it entwines with modern technology (Dr. G types up each prescription and prints it out for the patient to fill) and biomedicine.
Anthropologist Judith Farquhar describes clinical TCM as “knowing practice,” skillfully articulating the way that physiological-philosophical theories manifest in the mundane space of the clinical encounter. For me, this term captures the hidden profundity of TCM: that the sometimes-boring, sometimes-stuffy clinical room opens up onto centuries’ worth of history, philosophies of the body and the universe and the delicate harmonies that arise within them, and complicated entanglements between vastly different forms of knowledge. But all of this complexity pivots upon a deceptively simple goal: to help a sick patient become well.